Healthcare RCM Services
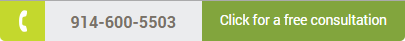
Revenue Cycle Management Services
EPHY Healthcare Solutions offers end to end Health Care Revenue Cycle Management(RCM) services for healthcare providers and clinics. Our primary goal is to maximize your cash flow with efficiency across the revenue cycle process.
We can improve your revenue by streamlining the front and back end processes through enhanced Revenue Management capabilities, domain exposure, and a healthy customized service delivery platform.
We showcase your Revenue Cycle flow by high level executive Dash Board reports that will give you a true picture of your practice cash flow in terms of projected collections and pending collectibles.
Medical Billing
EPHY Healthcare Solutions offers Quality Medical Billing & Payments processing services for Healthcare providers and Clinics.
Services Offered:
- Patient Registration
- Charge Capture
- Claims Submission
- Payment Processing
- Denial Posting
- Refund Processing
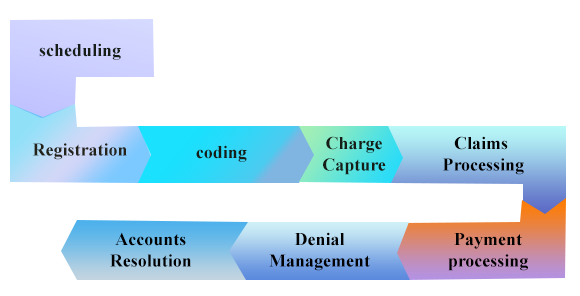
Patient Registration:
Our Medical Billing experts will capture the patient Demographics and insurance details in your medical billing system.
Solutions we offer
Benefits of EPHY Healthcare Patient Demographics
- In house software built with data capturing abilities
- Trained staff
- Quality Process
- Lower rejections
- Increase collections
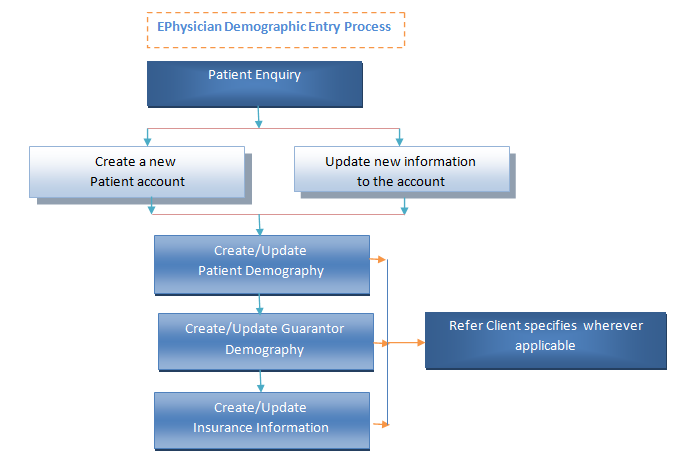
Charge Capture
Our charge entry experts will create appropriate charges in your system following the coding guidelines.
EPHY Healthcare Charge Capture Process
- Charges are captured in the billing system based on client’s specific guidelines
- We verify the patient eligibility for all the new patients before processing the charges in the billing system
- Charges that were held are sent to the client on a daily basis
- The charges entered are audited by our Quality team following client specific instructions and billed as a clean claim to the insurance companies
Benefits of EPHY Healthcare Charge Capture Process:
- Charge Entry on multi speciality practices
- Tracking the batch status through our Charge Control Log
- Efficient Quality Audits – Verification of all claims before claims submission there by resulting in increasing the Clean Claims percentage
- The charges entered are audited by our Quality team following client specific instructions and billed as a clean claim to the insurance companies
- Quicker Turnaround time
- Our staff is trained on CPT/HCPS code and Modifier validation
- HIPAA Complaint Process
Claims Submission
We at EPHY Healthcare Solutions submit your electronic claims directly to the payers, or based on your interest will utilize a third party clearing house to submit your electronic claims.
Benefits of EPHY Healthcare Electronic Claims Submission
- Easy transformation from paper based to Electronic submission
- Expertise working with different clearing houses
- Ensure the claims are verified through automated as well as manual edits for completeness before submitting it to the payers
- Round the clock access to the claim status reports
- Every single claim goes through the payer specific rules engine to zero out any payer rejections
- Payments are released within 15 to 20 business days of submission
- High level Dash Board reports
- Minimize the Data Entry Errors
- Increase in cash flow of the practice
- Better control & Improved Accuracy rates
- Claims are submitted electronically within 24 hours of meeting a patient
- Expertise working with the clearing house & payer front end rejection code sets, thereby resulting in quicker submission of claims
- We work 24/7 so there is no time lag in submitting the corrected claims to the insurer
Payment Processing
At EPHY Healthcare we receive the payments from the payers through ERA’s & Paper EOB’s. Our Payment processing executives will login to the clearing house web portal and download the ERA’s regularly. Alternatively, the paper EOB’s will be downloaded from our secured FTP server on frequent intervals.
Our highly skilled payment posting executives will post the insurance payments and capture the denials in the appropriate patient accounts by maintaining high level of accuracy and confidentiality
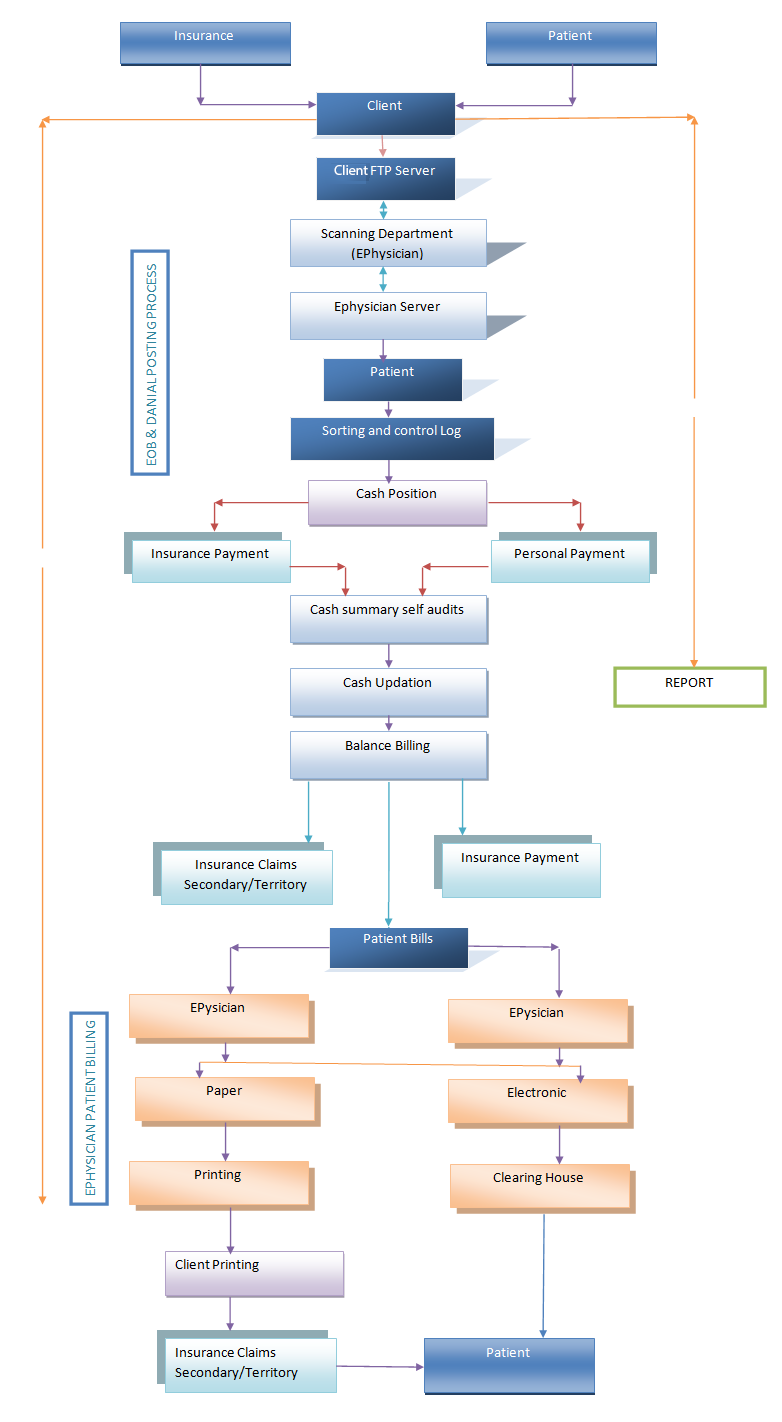
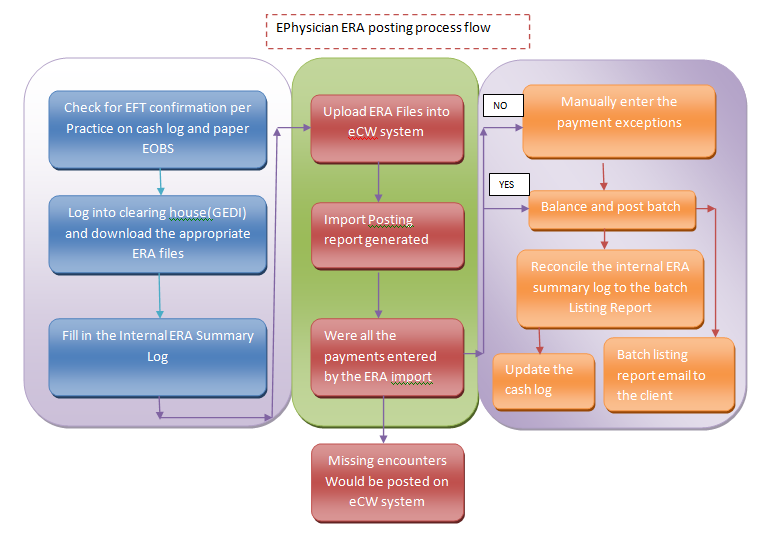
Payment Posting process at EPHY Healthcare Solutions
- Insurance ERA & EOB Postings
- Self-Pay payments posting & Patient Billing
- Processing Refunds/Overpayments
- Denials posting
Benefits of EPHY Healthcare Payment posting process
- Tracking the payment batches through our Payment Posting tracker
- Self-Pay payments posting & Patient Billing
- Payments applied in the system within 24-48 hours from the time of issue
- Upfront cost savings
- Automated payment posting engines for quicker postings
- Customizable Dashboard Reports like Transaction report (Number of line items received Vs posted), Un-posted transactions Report etc
Quality Process at EPHY Healthcare Solutions
EPHY Healthcare Solutions has a robust audit team which focus on reducing the insurance rejections and under payments and substantially increase the revenue of the healthcare provider.
Our Quality Assurance team has a pre-defined check list and verify the important fields in the demographics & charge entry like patient name, DOB, SSN#, policy id, DOS, referring physician, CPT, ICD & modifier combinations for accuracy. This process will eliminate 99% of the errors and then the claims are submitted electronically to the insurance companies.